Podiatric Care for Ankle Sprains

An ankle sprain occurs when the ligaments that support the ankle stretch or tear, usually due to sudden twisting or rolling of the foot. Inversion sprains happen when the foot rolls inward, affecting the outer ligaments, while eversion sprains involve the foot rolling outward, impacting the inner ligaments. Common causes include sports injuries, uneven surfaces, or missteps. Symptoms include pain, swelling, bruising, and limited mobility. Among the risk factors are poor footwear, weak ankle muscles, and previous sprains. A podiatrist can assess the severity of the sprain, provide imaging, if needed, and develop a treatment plan that may include rest, bracing, or specific stretches and exercises. If you experience ankle pain or instability, it is suggested that you consult a podiatrist for expert care and recovery guidance.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Susan Yeager, DPM from Yeager Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our office located in Redding, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Diabetic Foot Ulcers and Podiatric Care
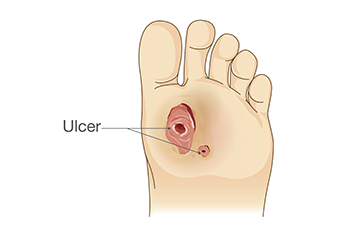
Diabetic foot ulcers are open wounds or sores that typically develop on the bottom of the foot in diabetics. They are caused by a combination of poor circulation, nerve damage, and repetitive pressure or injury to the foot. Risk factors include long-term diabetes, smoking, poorly controlled blood sugar, and improper footwear. Symptoms may include redness, swelling, drainage, or a foul odor. These ulcers can become infected and lead to serious complications. A podiatrist plays a key role in managing diabetic foot ulcers by providing wound care, pressure relief, and guidance on foot hygiene. If you have diabetes, it is strongly suggested that regular visits to a podiatrist are part of a routine plan that can help you to manage existing foot ulcers.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Susan Yeager, DPM from Yeager Foot and Ankle Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Redding, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Causes and Types of Corns

Corns are thickened areas of skin that develop in response to repeated pressure or friction, often from wearing ill-fitting shoes or abnormal walking patterns. They typically form on the tops and sides of toes or on the soles of the feet. Common causes include wearing tight footwear, high heels, or walking without proper support. There are different types of corns, including hard corns, soft corns found between the toes, and seed corns which appear on the bottom of the foot. While small corns may not cause pain, larger ones can become uncomfortable or lead to further irritation. A podiatrist can identify the cause, safely remove corns, and recommend footwear or custom orthotics to relieve pressure and prevent recurrence. If you have developed a corn, it is suggested that you confer with a podiatrist who can offer effective relief and treatment solutions.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Susan Yeager, DPM of Yeager Foot and Ankle Center. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Redding, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
Keep Your Feet Healthy So You Can Stay Active
Understanding Reconstructive Foot Surgery

Reconstructive foot surgery is performed to restore the shape and function of the foot when bones, joints, or soft tissues have been damaged due to trauma, disease, or deformity. Common causes include serious injuries, birth defects like clubfoot, infections, or complications from diabetes and vascular disease. A podiatrist may recommend reconstructive foot surgery when the anatomy of the foot is severely affected and conservative options are no longer effective. Procedures may involve removal of dead or infected tissue, skin grafts, or the use of tissue flaps that include skin, muscle, or bone. Tendon transfers and lengthening may be used to improve foot movement. In some cases, loss of limb may be discussed when reconstruction is not appropriate. Not everyone is a candidate for this surgery, particularly those with widespread infection, severe circulation problems, or poor overall health. A podiatrist can help determine whether surgery is appropriate and explain the options. If you are a candidate for reconstructive foot surgery, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Susan Yeager, DPM of Yeager Foot and Ankle Center. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Redding, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
Foot and Ankle Issues That Develop Without Injury

Many foot and ankle conditions can occur without a specific injury. These problems often result from gradual changes in foot structure, genetics, underlying health conditions, or daily habits. Common examples include bunions, hammertoes, and flat feet, which may form over time due to inherited traits or improper footwear. Plantar fasciitis and heel spurs can develop from repetitive strain or standing for long hours. Arthritis in the joints of the toes or ankles may cause stiffness, swelling, and reduced mobility as part of the aging process. Nerve disorders like peripheral neuropathy and tarsal tunnel syndrome can also affect the feet, even without trauma. Circulatory issues like peripheral arterial disease may lead to foot pain, slow-healing wounds, or changes in skin color. If you notice discomfort, numbness, or changes in your feet or ankles that are not related to an injury, it is suggested that you visit a podiatrist for a complete evaluation.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Susan Yeager, DPM from Yeager Foot and Ankle Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Redding, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.